The group of infectious diseases includes fungus on the feet, which is a type of mycosis. This pathology is caused by microscopic fungi. Nail plate disease is called onychomycosis.

Fungal lesions on the feet
This is a very common condition in both men and women. The most common types of mycosis are:
- trichophytosis;
- candidiasis;
- epidermophytosis.
Some fungi can infect animals and humans. It is necessary to know not only what is mycosis, but also why it develops. The main mechanism of human infection is contact. It is realized in direct and indirect ways. In the first case, the fungus infects the feet when in contact with soil, plants or sick people. Family infections have been reported.
Indirect pathogen transmission occurs when in contact with animal care items and patient personal belongings. These can be shoes, towels and scissors, as well as bath accessories.
Often the shipping factors are socks, stockings and other personal items. Foot fungus can develop after visiting public baths and swimming pools. This process involves the skin of the feet and the nail plate.
Contributing factors are:
- increased foot sweat;
- the presence of corns and abrasions;
- wear tight shoes;
- not adhering to personal hygiene;
- wearing other people's shoes;
- accommodation in hostels;
- weakened immunity;
- poor nutrition;
- the presence of other skin diseases;
- hypovitaminosis;
- alcohol addiction;
- smoking;
- walking barefoot;
- endocrine disorders.

Weak people tend to face this problem.
Common clinical manifestations
Fungus on the soles of the feet and nails can go unnoticed for a long time. With this disease, the following symptoms are observed:
- peeling skin;
- drought;
- the presence of diaper rash;
- thickening of the skin and nail plates;
- brittle nails;
- redness;
- itching;
- blooms white or yellowish;
- the presence of erosion;
- skin disease.
The fungus on the feet looks different. It all depends on the type of pathogen and the underlying disease. Sometimes an unpleasant smell leaves a person. Fungus on the feet does not cause deterioration of the general condition. Symptoms of poisoning are absent, as fungi are conditionally pathogenic microbes and are localized in the surface layer of the skin.

One foot is hit first. Then the fungus is introduced to the second limb. Often, the following areas are involved in the process:
- back of legs;
- distance between 4 to 5 fingers;
- nail plate.
Depending on the clinical signs, forms of squamous, dyshidrotic and intert Originous disease are distinguished. In the first case, scales appear on the reddened skin. Peeling is observed. Itching is an intermittent sign. He did not disturb all the patients. With dyshidrotic forms of mycosis, bubbles appear in the fornix. They can grow big. After a few days, they opened. Erosion appears in their place. Diaper rash appears. As the erosion dries, exfoliation is observed.
If the fungus on the skin of the feet is encrypted by a bacterial infection, the exudate becomes purulent. Pain appears. Fever is possible. Fungal infections sometimes provoke the development of interrelated mycosis. Its main feature is the presence of cracks with white rims. Oozing develops over time. Pain appears. Forms of erosion in crack areas. This form of the disease occurs in a chronic form with exacerbation in the summer.
Development of foot onychomycosis
Along with fungus on the feet, onychomycosis can be found. Thus, the nail is involved in the process. The prevalence of this pathology among the population is 10-20%. In recent years, the incidence of the disease in children has increased. The fungus grows actively and multiplies not only on the skin, but also on the nail plate.
People with varicose veins, hyperhidrosis, flat feet and endocrine diseases often face similar problems. The fungus multiplies inside the nail, gradually causing its destruction. If the disease is not cured, then it can last for years. The end result is nail release. Hyperkeratosis is common.
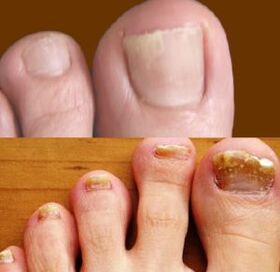
Distinguish between hypertrophic, normotrophic and atrophic onychomycosis. In the first case, the nails are dull and thickened. With atrophy, the color of the plate changes to brown. The detachment was noticed. With normotrophic onychomycosis, the shape and size of the nail do not change. With the development of onychomycosis of the feet, the following symptoms are observed:
- decreased nail density;
- change its color;
- the presence of white or yellow spots;
- itching;
- cracked skin;
- peeling;
- plate thickening;
- increased fragility.
If nail fungus treatment is not carried out, then there is a risk of developing paronychia. In this condition, purulent inflammation of the nails occurs.
Examination and treatment tactics
You need to know not only how the fungus starts in the feet, but also how to get rid of it. The therapy regimen is determined by the attending physician. Prior to that, the following studies will be required:
- inspection with Wood lamp;
- scrap microscopy;
- general clinical analysis;
- sowing on nutrient medium.

Differential diagnosis is made with psoriasis, onychodystrophy, lichen planus, congenital pachyonychia, trauma and eczema.
Every experienced dermatovenerologist knows how to treat toenail fungus. Antifungal drugs are used in the form of solutions, creams and varnishes.
Foot fungus treatment often involves surgery. Affected nails are removed.
With long -term epidermophytosis, systemic medications for foot fungus based on miconazole or ketoconazole may be prescribed. Proper treatment will kill germs. There are products on sale that fit the aisle of the affected nail plate. They come in the form of patches.
To increase the effectiveness of skin fungus treatment on the feet, vitamins, antibiotics (in case of secondary infections) and various ointments based on zinc and salicylic acid are prescribed.
You also need to follow a few rules:
- Feet should be washed daily.
- Change your socks more often.
- After the therapy is over, old things should be discarded.
- Socks, tights and stockings should be washed in a separate basin.
- When fungus is found on the feet, treatment will be successful if closed slippers are worn.
At the end of therapy, a scraping control study was performed.
























